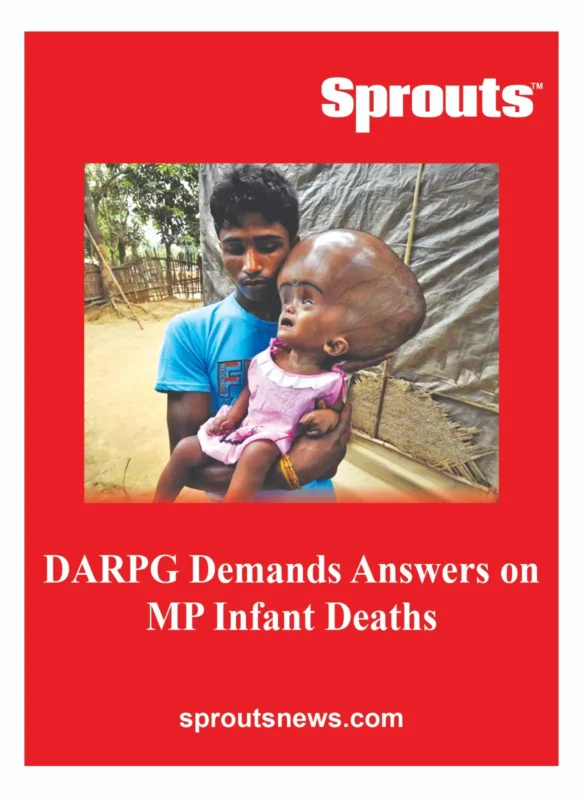
DARPG Demands Answers on MP Infant Deaths
• NHM Officials Under Scanner: Mangla, Sidhu, Sadana Named
• Systemic Neglect in MP Healthcare Exposed
• MP’s Tribal Healthcare Crisis: Why Are Infants Dying?
Madhya Pradesh faces a severe infant mortality crisis with an IMR of 43. Despite a 2014 mandate, the state bars general surgeons from emergency procedures, keeping FRUs dysfunctional. DARPG has now demanded accountability from NHM officials Harsha Mangla, Rajinder Sidhu, and Saloni Sadana for systemic failures affecting tribal communities.
- DARPG Demands Answers on MP Infant Deaths
- • NHM Officials Under Scanner: Mangla, Sidhu, Sadana Named
- • Systemic Neglect in MP Healthcare Exposed
- • MP’s Tribal Healthcare Crisis: Why Are Infants Dying?
- Madhya Pradesh Infant Deaths Crisis: DARPG Demands Accountability from NHM Officials
- Systemic Neglect of 2014 Health Mandate Worsens Tribal Healthcare Crisis
- Stalled Progress: High Mortality Persists Despite NHM Improvements
- Deep-Rooted Barriers: Anemia, Surgical Gaps, and Accountability Failures
- DARPG Intervention Spotlights Central and State NHM Leadership
- Editorial Stand: NCPCR Must Take Suo Motu Cognizance of Child Rights Violations
Click Here To Download the News Attachment
Madhya Pradesh Infant Deaths Crisis: DARPG Demands Accountability from NHM Officials
A Sprouts News Investigation Team (SIT) Exclusive reveals a systemic failure in Madhya Pradesh’s healthcare apparatus, linking soaring infant mortality rates directly to the non-implementation of a critical 2014 central policy. Despite an Infant Mortality Rate (IMR) of 43 per 1,000 live births in rural areas—far exceeding the national average of 28—state health authorities have consistently barred general surgeons from performing emergency procedures, leaving First Referral Units (FRUs) dysfunctional. The Department of Administrative Reforms and Public Grievances (DARPG) has now escalated the matter to the Union Health Ministry, demanding immediate corrective action and accountability from National Health Mission (NHM) officials.
This intervention follows a series of unresolved public grievances and petitions highlighting preventable deaths in tribal regions. The Sprouts News Investigation Team (SIT) has tracked how the state’s refusal to train general surgeons for emergency Caesarean sections has created a critical gap in care for high-risk mothers. The DARPG’s directive, issued on September 15, 2025, explicitly names Dr. Harsha Mangla (Director, NHM Division I), Rajinder Singh Sidhu (Under Secretary, NHM Division I), and Dr. Saloni Sadana (State Director, NHM Madhya Pradesh) to furnish action taken reports.
Systemic Neglect of 2014 Health Mandate Worsens Tribal Healthcare Crisis
In 2014, the Union Health Ministry issued binding Technical and Operational Guidelines to address India’s obstetrician shortage. This policy specifically mandated the training and empowerment of general surgeons to perform life-saving emergency Caesarean sections and manage obstetric complications in rural and tribal areas. The goal was to ensure that First Referral Units (FRUs) could function as intended, providing comprehensive emergency obstetric care.
However, NHM Madhya Pradesh has systematically sidelined this directive. Our investigation found that the state’s recruitment policies continue to prohibit general surgeons from conducting these procedures, rendering numerous FRUs clinically dysfunctional. This failure forces expectant mothers from tribal communities to undertake perilous journeys to distant facilities, often with fatal delays. Evidence uncovered by our team indicates that at least 35 Presidential petitions on this specific issue have been dismissed without meaningful action, despite a documented rise in adverse outcomes.
Also Read: Railway Transfer Scandal: Union Leader’s Rajendra Gujre 20-Year Grip at Kalyan.
Stalled Progress: High Mortality Persists Despite NHM Improvements
Over the past two decades, Madhya Pradesh has demonstrated measurable, albeit uneven, progress under the National Health Mission. Institutional delivery rates have soared to over 90%, postnatal care coverage has seen a dramatic increase from 2% to 88%, and C-section rates have risen from 4% to 13% since the early 2000s. These metrics traditionally indicate improved healthcare access and utilization.
Yet, the state’s neonatal and infant mortality figures remain alarmingly stagnant. The rural IMR of 43, compared to 28 in urban areas, exposes a deep urban-rural divide. The most devastating impact is concentrated among the poorest households and tribal communities, indicating that systemic inequities are overriding nominal gains. This disparity suggests that while basic services have expanded, the quality and emergency responsiveness of care have not kept pace, particularly in high-need regions.
Deep-Rooted Barriers: Anemia, Surgical Gaps, and Accountability Failures
The crisis extends beyond maternal care to encompass pervasive child health challenges. Our review identifies several persistent, unaddressed barriers contributing to the high mortality burden. Maternal anemia continues to affect a staggering 60% of women, a rate that has shown little improvement over two decades, compromising both maternal and infant health from birth.
Furthermore, children in tribal regions are routinely denied essential emergency surgical procedures. Recruitment restrictions on general surgeons mean lifesaving interventions like hernia repairs, torsion testis surgery, and neonatal circumcisions are inaccessible. This critical gap in pediatric surgical care represents a severe violation of child health rights. Despite improvements in social determinants like literacy and sanitation, the state’s failure to address these specific medical and systemic flaws has prevented social gains from translating into survival outcomes.
Related Article : 3,200 Mothers Dead as Madhya Pradesh Defies 2014 Health Mandate.
DARPG Intervention Spotlights Central and State NHM Leadership
The DARPG’s September 2025 Office Memorandum marks a potential turning point, applying formal pressure on the health bureaucracy. The memorandum explicitly directs the Union Health Ministry to align with CPGRAMS grievance redressal norms and establish a clear framework for accountability. This action formally places the onus on both central and state-level NHM leadership to explain the policy paralysis.
For the first time, a central government body has officially drawn a direct line between Madhya Pradesh’s discriminatory NHM recruitment rules and the preventable deaths of infants and mothers. This acknowledgment validates long-standing concerns raised by healthcare advocates and citizens, shifting the issue from administrative neglect to a matter of mandated accountability. The performance of officials Dr. Harsha Mangla, Rajinder Singh Sidhu, and Dr. Saloni Sadana is now under unprecedented scrutiny.
Editorial Stand: NCPCR Must Take Suo Motu Cognizance of Child Rights Violations
Sprouts News joins Editor-in-Chief Unmesh Gujarathi in demanding immediate action. The National Commission for Protection of Child Rights (NCPCR) must take suo motu cognizance of this grave crisis. The deliberate exclusion of general surgeons from emergency care teams is not merely an administrative failure; it is a direct violation of the right to health and life for India’s most vulnerable children and mothers.
This policy failure disproportionately endangers tribal communities, exacerbating existing healthcare disparities. The Sprouts News Investigation Team will continue its oversight of this case, ensuring that the voices of these communities are heard at the highest levels of governance. We call for immediate corrective action to operationalize all FRUs and enforce the 2014 guidelines without further delay.